Brachial plexus Injury
Brachial plexus
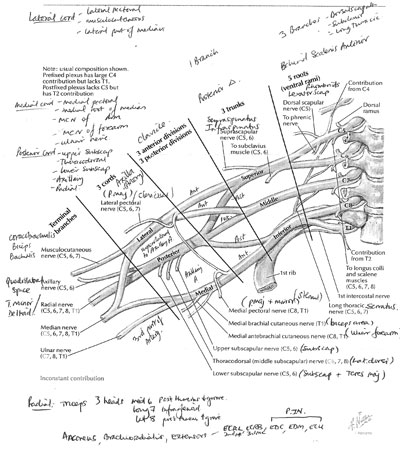
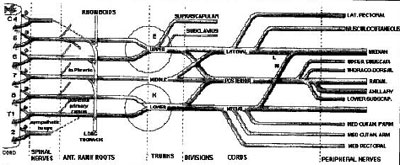
Sequence (mnemonic): Robert Taylor Drinks Cold Beer (Rami, Trunks, Divisions, Cords & Branches)
Positions:
The roots and trunks lie in the posterior triangle of the neck.
The divisions are deep to the clavicle .
The cords are posterior to the pectoralis minor
Terminal branches begin in the axilla .
Roots (5)
Are formed by the ven
tral rami of spinal nerves C5 - T1.
Trunks (3)
The 5th and 6th cervical roots join to form the upper trunk .
The 7th cervical root forms the middle trunk .
The 8th cervical and 1st thoracic roots join to form the lower trunk .
Divisions (6)
Each trunk divides into an anterior and a posterior division.
Cords (3)
The three posterior divisions join to form the posterior cord (C5-T1)
The anterior divisions of the upper and middle trunk unite to form the lateral cord (C5-C7).
The anterior division of the lower trunk continues alone as the medial cord (only C8-T1).
Branches
Branches come from the rami, the trunks and the cords; usually no branches from the divisions.
Branches from Roots
Phrenic nerve (C5)
Dorsal scapular nerve (C5) innervates rhomboids and levator scapulae.
Long thoracic nerve (C5,6,7) serratus anterior.
Branches from Trunks (2 both from upper)
Nerve to subclavius (C5,6)
Suprascapular nerve (C5,6) - Supraspinatus and Infraspinatus and shoulder innervation.
Branches from Cords
Lateral Cord
Lateral pectoral nerve (C5,6,7) pectoralis major (clavicular head) and minor.
Posterior Cord
Upper subscapular nerve (C5,6) upper subscapularis.
Lower subscapular nerve (C5,6) lower subscapularis and teres major.
Thoracodorsal nerve (C5,6,7) Latissimus dorsi.
Medial Cord (all from lower trunk C8, T1)
Medial pectoral nerve (C8,T1) pectoralis major and minor.
Medial cutaneous nerve of arm (C8,T1) medial portion of the arm.
Medial cutaneous nerve of forearm (antebrachial cutaneous) (C8,T1) medial half of the forearm.
Terminal Branches
From lateral cord (C5-7)
Musculocutaneous nerve (C5,6,7) later gives the lateral cutaneous nerve of forearm.
Lateral root of the median nerve (C5,6,7)
From posterior cord (All roots)
Axillary nerve (C5,6)
Radial nerve (C5,6,7,8,T1)
From medial cord (C8-T1)
Medial root of Median nerve (C8,T1)
Ulnar nerve (C7,8,T1) - variable C7 root from ramus or lateral cord.
Aetiology of Brachial Plexus Injury
Birth
Motorbike RTA's most common, 80 % have other severe injuries (Axillary or sublavian artery in 20%)
Also humerus, scapula, rib fractures and shoulder dislocation
Classification
Upper Erbs
Lower Klumpkes
Lefferts classification:
Open or Closed (traction) injuries
A. Supraclavicular
Supraganglionic (Intradural root avulsions)
Infraganglionic (Root or trunk injury)
Or,
Complete
Intradural C5-T1 = 1/6th
Combined intra and extradural 1/3rd
Incomplete 50% - mainly upper trunk (C5 and C6)
B. Infraclavicular
C. Postanaesthetic palsy
D. Radiation injury to the brachial plexus
E. Obstetric palsy
Diagnosis
Preganglionic intraspinal lesions vs postganglionic extraspinal lesions
Cutaneous axon reflexes - histamine scratched into area of skin that the nerve supplies
Normal response - cutaneous vasodilatation and wheal formation (nerve), flare response (axonal)
Preganglionic disruption of nerve- anaesthesia, but normal axonal response (flare)
Postganglionic disruption of nerve- anaesthesia, vasodilatation and wheal formation but flare absent.
Root avulsion from spinal cord
Pain from avulsions - shooting or crushing/burning (deafferentation) ½ < 1/7, most < 2/52.
Upper preganglionic (lesion proximal to long thoracic and dorsal scapular nerves)
Long Thoracic nerve - serratus anterior - winging of scapula
Nerve to Rhomboids - retropulse shoulder or hand from behind
In lower plexus (proximal to Sympathetic ganglion)
Horner's syndrome - pupil constriction (miosis), sunken eye (enopthalmos), upper eyelid droop (ptosis) and ipselateral loss of sweating on face (anhydrosis). Can occur elsewhere (brainstem - demyelination, CVA), Cord (syringomyelia), thoracic outlet (Pancoast's Tumour) or on Int. Carotid Artery (Aneurysm)
Examination
Observe for bruising,abrasions and Horner's syndrome. Swelling in neck ?CSF leak.
Tinel's sign for postganglionic injury.
Area of sensory deficit - draw the distribution on a diagram.
Joint stiffness or contractures - negate tendon transfers and make exam difficult.
Motor power : Start proximal to distal.
In obstetric brachial plexus palsy:
Ipsilateral foot may be small due to hemicord injury.
Shoulder may be subluxed due to internal rotation deformity of subscapularis.
Upper plexus (Erb's - waiters tip deformity C5,C6 +/- C7)
Limb extended at elbow, flaccid at side of trunk, adducted, internally rotated.
Loss of Shoulder Abduction (deltoid, supraspinatus), External rotation (infraspinatus and teres minor)
Elbow flexion (biceps, brachialis, brachioradialis)
Supination (supinator)
Sensory Loss : Over deltoid, lateral aspect of forearm and hand.
Caused by shoulder down injury.
Lower plexus (Klumpkes C8, T1 +/- C7)
Weak intrinsics of hand, paralysis of wrist and finger flexors
Sensory deficit over medial aspect of arm forearm and hand.
Caused by Shoulder up injury (difficult births, falls onto the outstretched arm, crutches)
Investigations
Plain films: CXR high diaphragm from Phrenic nerve injury.
C-Spine - transverse process and 1st rib fractures
CT Myelogram and MRI can demonstrate avulsion of roots.
Neurophysiology
Can be complex in acute situation. Need expert interpretation.
EMGs at 3-4 weeks after injury to determine extent of injury (after Wallerian degeneration)
Demonstration of denervation potentials in the segmental paraspinal muscles from posterior rami
Treatment
ATLS- treat life or immediate limb threatening injury (major vessel)
Indications for early exploration +/- repair
Open Injuries (+ repair if wound clean)
Vascular injury (get arteriography) preferably single op for repair of artery and nerves.
High energy injuries referral to specialist unit
Progressive Neurology
Complete Lesions of any part of plexus
Incomplete or low energy Injury : Document neurology and perform neurophysiology if no improvement and consider exploration at 2-3 months.
Contraindications to exploration
Other life threatening injuries in patient. Outcome is worse and surgery harder after 2-3 months.
Surgical goals
Establish extent of neurological injury
Preserve function by repair, neurotization (nerve transfer) or neurolysis.
Restore function by palliative reconstruction.
Operative Technique
Incision depends on supra- or infra-clavicular. May need to osteotomise the clavicle if both.
Use intraoperative nerve stimulation (SSEP's)
Primary nerve repair (neurorrhaphy) if nerve action potential and no tension.
Neurolysis for scar tissue
Nerve grafting (Neurotization)
For root avulsions of upper plexus if nerve integrity lost or no nerve action potentials
e.g. Accessory to Suprascapular for shoulder function.
Intercostal nerve (or ulnar fascicle) to musculocutaneous nerve to gain elbow flexion.
Sensory Nerves (Medial/Lateral cutaneous nerves of forearm, Medial cutaneous nerve of arm, Superficial radial, Intercostobrachial)
? Reimplantation of avulsed roots for complete lesion (Hemilaminectomy). C/I if cord injured
Results do appear better for early repair/ reconstruction
Post op
Splintage of shoulder for 6/52.
Physiotherapy to keep joints mobile
Pain management until reinnervation (medication and nerve blocks)
Wait 12-18 months to determine amount of regeneration, depending on advancing Tinel's sign.
Salvage procedures
Tendon transfers eg. Trapezius to deltoid for abduction of shoulder
Latissimus dorsi transfer to posterior cuff (for external rotation of shoulder)
Pectoralis Minor transfer to biceps (with Palmaris longus interposition graft).
Hand function restored by standard transfers.
Joint fusions - Eg. Shoulder fusion useful if scapulothoracic function preserved. Amputation (rare)
Spinal accessory nerve
Anatomy Superficial in the posterior cervical triangle, supplies sternocleidomastoid and trapezius (also has cervical plexus innervation).
Causes of injury penetrating injuries to the neck, lymph node biopsy, radical neck dissection
Clinical findings Aching of shoulder, wasting of upper trapezius, shoulder sag, weakness of shoulder girdle and scapular dysrythmia.
Treatment Primary or delayed suture or interfascicular nerve graft.
Results should be good as primarily a motor nerve
|
